New Study Reveals Genetic Link Between Schizophrenia and Osteoporosis
|
General Studies Paper II: Health |
Why in News?
Recent genomic research has uncovered a surprising shared genetic architecture between schizophrenia and osteoporosis (porous bones), showing that these seemingly unrelated conditions may be biologically connected at the DNA level.
Highlights of Recent Genetic Study
- Studied By: The landmark research of link between schizophrenia and osteoporosis was led by Dr. Feng Liu and colleagues at Tianjin Medical University General Hospital and published in Genomic Psychiatry. It integrated expertise in psychiatric genetics, bone biology, and bioinformatics.
- Samples: The analysis drew on over 500,000 individuals’ genome-wide data, including schizophrenia genetic information from the Psychiatric Genomics Consortium and six osteoporosis-related traits measured across skeletal sites such as heel, lumbar spine, femoral neck, and total body BMD. Sample sizes for bone traits ranged up to about 426,824 participants for some measures.
- Method Used: Researchers employed a multi-level genomic framework that combined global polygenic overlap, local genetic correlations, and conditional/conjunctional false discovery rate (cond/conjFDR) analyses to uncover shared genetic variants between the two conditions.
- Findings:
-
- The study identified 195 shared genetic loci mapping to 1,376 protein-coding genes, indicating a substantial genetic overlap between schizophrenia and osteoporosis-related traits.
- Schizophrenia and heel BMD showed the strongest shared genetic architecture, with 329 trait-influencing variants in common.
- A key discovery was the mixed effect patterns: only about 21 % to 68 % of shared variants had concordant impacts on both traits, meaning some variants increased schizophrenia risk while decreasing bone density, and vice versa.
- Shared genes cluster in pathways related to organonitrogen compound metabolism, anatomical structure development, and biological regulation, suggesting common biological systems linking neuropsychiatric and skeletal health.
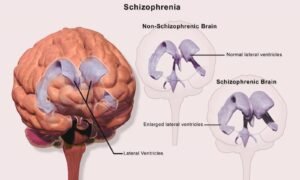
What is Schizophrenia?
- About: Schizophrenia is a severe, chronic psychiatric disorder that affects how a person thinks, feels, and behaves. It alters perception of reality, often leading to psychosis. It is a complex brain-based illness involving disturbed cognition and emotional regulation.
- Classification: Schizophrenia is classified under psychotic disorders in diagnostic systems such as DSM-5-TR and ICD-11. It is associated with reduced life expectancy by 10–20 years, mainly due to cardiovascular disease and suicide risk.
- Risk Factors: The disorder arises from a combination of genetic vulnerability and environmental triggers. Large genomic studies show schizophrenia is highly polygenic, involving hundreds of genetic variants. Environmental factors include prenatal infections, obstetric complications, cannabis use during adolescence, urban stress, and childhood trauma.
- Symptoms: Symptoms are grouped into positive, negative, and cognitive categories.
- Positive symptoms include hallucinations, delusions, and disorganized speech.
- Negative symptoms involve emotional withdrawal, lack of motivation, and reduced speech output.
- Cognitive symptoms include poor attention, memory deficits, and impaired executive function.
- Severity: According to the World Health Organization (WHO), it affects about 24 million people globally, or roughly 1 in 300 individuals. Around 20–30% of patients achieve substantial recovery with treatment, while others require long-term care. Approximately 5–10% of individuals die by suicide, particularly in early stages.
- Treatment: Treatment combines antipsychotic medications, psychotherapy, and community support. Second-generation antipsychotics such as risperidone, olanzapine, and aripiprazole target dopamine pathways to reduce psychosis. Cognitive Behavioral Therapy (CBT) and family therapy enhance coping skills.
How Brain Disorders Influence Bone Metabolism?
- The brain and skeleton communicate through a dynamic neuro–skeletal axis. The hypothalamus regulates bone remodeling via autonomic nervous signals and hormonal pathways. Bone is not inert tissue; it responds to central nervous system signals that influence osteoblast (bone-forming) and osteoclast (bone-resorbing) activity. Research shows that disruptions in brain signaling can alter bone turnover rates, affecting bone mineral density (BMD).
- Brain disorders frequently disturb the hypothalamic–pituitary–adrenal (HPA) axis, leading to sustained elevation of cortisol. Chronic high cortisol suppresses osteoblast function and enhances bone resorption. Patients with severe depression, schizophrenia, or chronic anxiety often exhibit altered cortisol rhythms.
- Key neurotransmitters such as dopamine, serotonin, and glutamate influence bone metabolism beyond the brain. Serotonin receptors are present in bone cells and regulate formation and resorption balance. Dysregulation of these neurotransmitters in neurological or psychiatric disorders may therefore disturb bone turnover.
- Many brain disorders involve chronic low-grade inflammation. Elevated cytokines such as IL-6, TNF-α, and IL-1β accelerate osteoclast activity and bone breakdown. Neuroinflammation can spill over into systemic circulation, creating a pro-resorptive environment. Persistent inflammatory signaling reduces bone strength over time.
- Brain disorders often impair physical activity, nutrition, and sunlight exposure, all essential for bone health. Reduced mobility lowers mechanical loading on bones, weakening structural integrity. Poor dietary intake decreases calcium and vitamin D levels. Neuromuscular dysfunction also increases fall risk, compounding fracture probability.
Significance of the New Findings
- Translates Clinical Comorbidity: The discovery of 195 shared genetic loci between schizophrenia and osteoporosis moves the explanation of high fracture risk in psychiatric patients from epidemiological speculation to biologically grounded evidence, showing that bone fragility is partly rooted in genetic architecture rather than just lifestyle or medications. This improves clinical understanding of co‑occurrence mechanisms.
- Enables Genetic Risk Stratification: With 1,376 protein‑coding genes mapped to shared regions, clinicians and researchers can develop polygenic risk scores (PRS) that integrate bone and psychiatric risk, guiding earlier monitoring and prevention for high‑risk individuals before clinical osteoporosis manifests.
- Bridges Organ Systems: The study highlights cross‑tissue genetic pathways linking the central nervous system and skeletal system, supporting a paradigm of organ‑system interconnectedness rather than siloed disease models. Such insights can inform interdisciplinary care models that simultaneously address mental and bone health.
- Drives Precision Therapeutics: Identifying shared biological pathways offers targetable molecular mechanisms for future drug development, enabling therapies that consider both brain and bone effects. It also encourages multi‑omics and trans‑ethnic studies to validate and expand findings across populations.